This is not a piece I ever thought I would write. This is not a story I ever expected to tell. It’s an October Breast Cancer Awareness Month feature about my friend, SoulCycle Master Instructor Stacey Griffith…
I have known Stacey Griffith for over 15 years, first as a rider in her class at SoulCycle. We became great friends too, kindred spirits in our love of sports, and travel adventure buddies. Stacey and I had big plans last summer, the launch of a Love & Sports branded content vertical on Style Of Sport, featuring editorial created for the apparel brand she co-founded with her partner Michelle Smith. But those plans got put on hold in an instant when Stacey received a diagnosis of breast cancer in June.
Stacey is one of the most popular SoulCycle teachers, one of the originals from SoulCycle’s inception with a devoted following. She is one of those special fitness instructors, who combine inspiration and motivation into a fun and addictive workout. Her class is an escape, for me and countless others, where for 45 minutes you forget about the world outside and leave your problems at the door. Stacey has coached and guided her students through many of those problems, real-life tough stuff. A number of women have gone through breast cancer with her in that room. The last thing anyone would imagine is that she would be on the receiving end of this disease. Nor would she.
I remember the day so well. It was a Friday. She and I were supposed to meet that afternoon. I rode her class that morning and confirmed I’d see her later. She was a bit non-committal, but I stressed we needed to meet if we were going to make our deadline for the Love & Sports launch. She told me she had to go get a mammogram. I said come over after. She said she was scared. I said we’re all scared of mammograms. They’re terrifying.
At about 1pm, I got a text from Michelle, Stacey’s partner and girlfriend: “Stacey’s not going to be able to make your meeting. She’ll fill you in later.” I knew this couldn’t be good. I texted Stacey and said I hope everything is okay. She wrote back “Not great”. I didn’t want to be pushy. I wanted to respect her privacy, but I sent a quick text saying I was around anytime if she wanted to talk.
Of course I was totally panicked. I had had a tiny breast cancer scare myself a few years ago. It thankfully turned out to be nothing, but I did have some sense of the fear and anxiety she might be experiencing. Stacey called me that Sunday and told me there was a large mass in her right breast. Her gynecologist had felt it a couple of weeks before and ordered the mammogram, so it wasn’t the routine annual we all get. She knew there was something wrong and that’s why she was scared.
And so began the process, the treatment for breast cancer that so many women go through. Stacey is being treated at The Dubin Breast Center of The Tisch Cancer Institute at Mount Sinai by Dr. Elisa Port and Dr. Amy Tiersten. She has just finished 12 weeks of chemotherapy. We got together a couple of weeks ago to talk about this first phase of treatment, how she’s doing physically and emotionally, and what’s next:
Claudia Lebenthal: I haven’t really seen you since this all began. I remember that weekend so well when you found out you had breast cancer. You spoke so calmly and rationally that Sunday as if it was happening to someone else. It was so strange and surreal.
Stacey Griffith: It was the first time I had ever gotten medical news about myself. From a sober state of mind, totally lucid and present, I physically disassociated from my own body. It was like I was a shell. I couldn’t feel anything. I couldn’t think anything. I couldn’t talk. I couldn’t make any decisions. The next morning when I was trying to process everything I just thought, ‘What am I going to do?’
CL: I remember you taught that Monday morning. I rode up on the podium and kept thinking, ‘How the hell is she doing this? How the hell is she faking it?’
SG: You were the only one who knew. What’s strange is one student who’s also at The Dubin Center going through a similar thing, and another student who had breast cancer and was also treated at The Dubin Center, were both in class together. They’ve never been together in that class. Of all the classes for them to be together… the one where I could barely keep it together.
CL: You would have never known.
SG: At the end of class they both came over to me. Geralyn pointed at Jamie and asked, “Can you believe how strong she is?”, not knowing about me. And Geralyn is one of my dear friends. I don’t know how I didn’t lose it at that moment. Jamie kind of knew because I had told her I was really nervous about going to get a mammogram. She looked at me, but there was this unspoken code of silence. But after that I could not go back in that room.
CL: You stayed on the schedule for a few weeks but kept subbing out your classes. Did SoulCycle know?
SG: I had told the CEO I was having some medical issues but I didn’t want the telephone chain going around. I wanted to be sure I had a plan before I let that cat out of the bag. Just a handful of us knew what was really going on.
CL: Then everyone got the email from SoulCycle on June 26. I remember imagining what the flood of responses must be, the texts, now that everyone knew why you hadn’t been teaching for the last month. People have wondered where you’ve been and that letter pops into their inboxes. We know what a dedicated following you have, and how much people love you, tell me about the immediate response.
………………………………………………….
Dear Friends,
As many of you have noticed I haven’t been on the SoulCycle schedule for a while, and I am writing to share why and also to make a sincere request.
Having been through a series of tests over the last couple of weeks, I was recently diagnosed with breast cancer. I cannot quite believe I am saying those words.
While devastating news to receive, here’s what I know with certainty: with the love and support of my friends, my family and my community I know that I am going to beat this.
I will be teaching in the Hamptons for the 4th of July weekend. You can see me there Friday 30th June – 4th July. We’re going to celebrate our time together, after which my treatment will commence. I’ll update you as and when I can thereafter.
Be assured I have the best team of medical professionals surrounding me and guiding me through this, and I have my family and loved ones to lean on. I hope you will understand my need for space and privacy through this journey, and know that you are in my heart always.
With love and soul, always. Stacey x
………………………………………………….
SG: It was awful.
CL: I didn’t expect you were going to say that.
SG: It was awful because it’s me. I’m not the one who’s supposed to get this. I’m supposed to take care of all of you guys. I don’t want to be babied. I don’t want to be chicken souped. This is not my role. Everybody had a doctor. Everybody had a friend. Everybody had a sister, or a mom, or them. It was so overwhelming. Imagine how many people I know, so many wonderful women.
CL: I know. And I’m sure everyone thinks they are just trying to help. Everyone wants to help.
SG: Everyone was just trying to make sure I was well taken care of. But the hardest part was I was just trying to have anonymity (laughs). But that wasn’t going to happen. I’ve been a bit of a recluse for the last 3 months. Phone, social media, and in person. It’s just been easier for me to stay in my little bubble.
CL: You’ve always done that though, knowing when to retreat when there was too much personal stuff going on. It’s hard when your job has you front and center, trying to be positive for everybody.
SG: I’ve never been that teacher who brings their personal life into the room. It’s definitely a style of teaching. They bring in their stuff that’s funny. They bring in their stuff that’s deep. They bring in their opinions. I’ve really tried not to be that teacher. But with this it’s kind of difficult, and that’s what made the 4th of July weekend so hard.
CL: I don’t know how you did it. The 4th of July weekend in the Hamptons at the SoulCycle Barn is such a packed weekend for your classes to begin with, the convergence of all your different studio followings in one place. From the second I saw that email, I thought about how every person who adores you, all your regulars, would want to be there and show you their love. And how insane that was going to be.
SG: That was probably the hardest teaching week of my entire career. I made it through 5 out of the 6 days. The last day I just couldn’t. I subbed that day out.
CL: Tell me about that first class.
SG: Oh my gosh… one of my students, a sweet guy who towers over me came up to me and he just broke down in tears in the first class. Then I had to teach another class with his compassion on my heart. I just thought, ‘How I am going to do this all week long?’ But my students are so important to me. That was the kickoff of summer, and I thought what a buzzkill. I didn’t want everyone to start their summer off with me bailing and not be there to say goodbye. I thought I owed it to them. I will have been there 17 years this October.
CL: And you taught like 3 or 4 classes a day for the next 5 days…
SG: As hard as they were, some of those classes were in the top ten of my teaching career. The last one, which no one knew was going to be my last one, was musically deep, musically pretty flawless as far as curation of songs… which was another really difficult thing to do. ‘How am I going to play this? I’m going to cry my way through that.’ It was so complex to choose the music. 28 songs a day times 5.
CL: So after that was when you started chemo, a very different kickoff to your summer…
SG: We had the most perfect summer rental. It was 90 seconds from the Barn. I was so excited to teach more than I had ever taught, and there I was so close and not teaching. Then I had to drive into the city for treatment once a week. I would get up at 5am and drive back the same day. I’d drive because I wanted to stay in my normal routine, normal cadence.
CL: And what is a day of chemo like? Can you describe what happens from start to finish, from when you walk into the hospital to when you leave.
SG: It would vary a bit, because every third treatment I would get immunotherapy which is a separate drip. My appointment was usually at 8:30 or 11am. I would get there and have to wait a little bit because they were always behind. There was always somebody like me, who got into treatment last minute that they had to see. They are so accommodating. There are only 12 rooms up at The Dubin Center, and only so many chairs in there. There’s no hierarchy either. It’s first-come, first-serve no matter who you are.
CL: Cancer doesn’t discriminate and neither do they.
SG: I would usually go in about 45 minutes after arrived and get access, which is when they put the IV into your arm. My dad’s tattoo, the G in his middle name, points directly to where they put it in every time — and he also had cancer. Everyone says chemo is the worst part, but for me it wasn’t. I think it’s because for the last 10 years, 4 times a year, I get IV Drips for my iron deficiency and for my anemia. So my body and my arm are used to this protocol.
CL: What was the protocol?
SG: First you have to get weighed and then they do bloodwork. You wait for your labs to come back, and unless they are perfect they don’t allow you to get chemo. That was the scary part. I only failed my labs once. I was so upset..
CL: So what are they looking for?
SG: On days I would have certain foods it would show up in my glucose level. On the first day I had three coconut waters thinking that was good for hydration, but my potassium was super jacked. They told me I had to come back later, but then I explained why. What I think they’re mostly worried about is your white blood cell count. I believe mine was always high because of exercise. I also tried to go into the ocean every day, to at least immerse myself in the salt water. Every morning I would wake up and take a cold Wim Hof style shower. No one was around so I would do weird wacky stuff. The sun would be shining. I felt like a 60s California hippie. I do think a lot of that works.
CL: What exactly do they put in those IV bags? How many bags do you go through? How long are you physically there with an IV drip in your arm?
SG: First there was a premed, which was just basically saline. It’s not part of the usual protocol but someone had suggested I do this. It kind of hydrates your body before you get chemo which was such a great tip. That would take about 10-15 minutes. Then they’d give me a steroid to help with the chemo-related fatigue. That would take about 30 minutes. Then there was the immunotherapy every third time. That was 90 minutes. And then the Tamoxifen. After that you have to get your vitals taken.
CL: And what were those ice bags I saw on your feet in a picture?
SG: They put your feet and hands on ice when they put in the Tamoxifen because it’s so intense and causes nerve damage, which I do now have in my feet. It’s neuropathy and very typical. The feeling will come back. You’ll laugh about this… at the first treatment, they give you Benadryl in case you’re allergic to anything. It knocks you out. I fell asleep for an hour with my mouth open, with ice on my hands and feet. When my friend and girlfriend came back they were like, ‘Oh my god is she dead??’ That bag takes about an hour with your hands and feet on ice and then you have to wait for your feet to unthaw so you can walk. I walked home every time, even when it was raining. I walked there too. I had to warrior through it, but typically I would take a 30-90 minute nap as soon as I got home.
CL: And that protocol stayed the same the whole time? I remember you saying to me I hope they still give me the steroid.
SG: Yeah they tried to take it away.
CL: Why would they want to take it away?
SG: They didn’t think I needed it anymore, but that was probably because it was working. I just didn’t want to jeopardize the energy it gave me. It was really quite magical and it would stay in my body until right when I would need it again. And it did help with getting my mind off this. How I dealt with this whole diagnosis was I just didn’t stop. I think that was one of the most annoying things for my family to deal with because I was up late at night. Sometimes I wouldn’t go to bed until 3am. And then I would get up early. But the rollercoaster of fatigue was hard to predict.
CL: Did you ever get used to the routine of all of this?
SG: The first day of my treatment, I had so much stuff people had given me. I packed like three bags to take with me. I had blankets, candles, crystals. I had imagined what it was going to be like. I didn’t realize I wasn’t really going to need anything except a blanket, and they had blankets there. By the last treatment I just showed up in one of my old SoulCycle sweatshirts. I had cut a hole so I didn’t have to take it off to give them access to my arm for the drip. Everyone thought that was so great. I’m obsessed with my nurses. I love them all. They all have nicknames. You know it’s like class. There was so much attention and care. They were so gentle and so amazing, but it was just so intense. I’m not used to being taken care of like that, having something wrong.
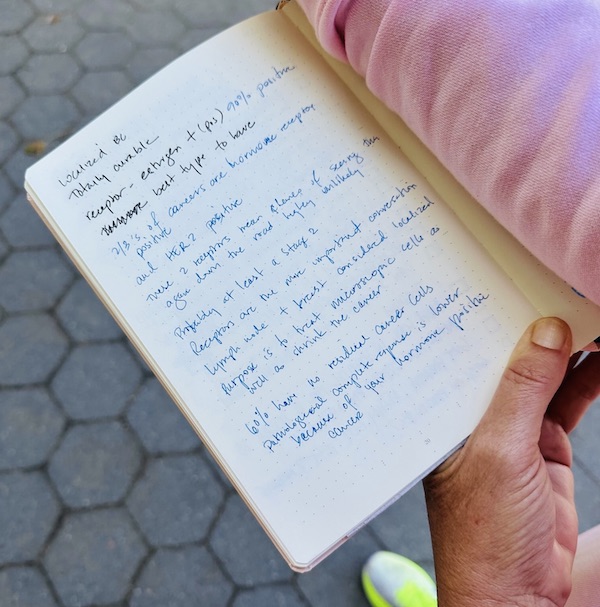
CL: So I want to ask you what type and where is the cancer you have in your body?
SG: I have HER2 positive. It is probably at least Stage 2. The good news is it’s totally curable (shows me her notes)
Totally curable… best type to have
2/3 of cancers are hormone receptor and HER2 positive. These 2 receptors mean chance of seeing them again down the road highly is unlikely
Receptors are the more important conversation
Lymph node + breast considered localized
Purpose is to treat microscopic cells as well as shrink the cancer
60% have no residual cancer cells. Pathological complete response is lower because of your hormone positive cancer
CL: Where is the cancer?
SG: Right breast and right lymph node. It was diagnosed via triple biopsy. It wasn’t my favorite part of this journey. I have had a life where I’ve never really had to go to the doctor for anything major. My ailments have all been injuries from teaching — physical, not health issues. They are work-related. They’ve been caused by me and by my job. This has been like an attack on my physical being I’ve had no control over.
CL: So we are chatting at this moment when you are officially done with the chemo. You were in a trial you said. Can you tell me a little bit about that?
SG: I didn’t really investigate it too much. You know I’m just such a jump-out-of-an-airplane sort of a girl. If you tell me the chute is going to open and I know you’ve been flying for 40 years, I’m going to trust you.
CL: Is it a new trial?
SG: It’s been around for about 2 years and they have been having great results. I told them I was going to be patient zero. You won’t have had anybody like me.
CL: From what I understand the goal of the trial is to avoid a mastectomy. Where are we now? For so many women that decision becomes a preemptive one.
SG: I’ve vacillated 3 to 4 times. Originally I said, “Just take them, I don’t want them. I don’t want it to come back. I don’t want any trace. I don’t want a mammogram every year.” With a bilateral mastectomy, you don’t have to have annual mammograms anymore. The idea of that seems smart, but the recovery is a long one. Right now the tumor is undetectable in the breast but they can’t see the lymph nodes. If there is no trace, they can go in and do a lumpectomy, take out the markers and what is left. Then I have 5 weeks of radiation. But if I get the lumpectomy and there are traces of cancer in my lymph nodes, I will have to get the mastectomy at a later date.
CL: So they’re letting the chemo cook right now, right? You finished last week but it keeps working even after you’re done as I understand. So we’re in a hovering pattern until after the radiation.
SG: Which I don’t want to do. The radiation is 5 weeks, Monday to Friday, once a day, every day. I just don’t want to lose my hair again.
CL: Radiation makes you lose your hair? I thought it was the chemo.
SG: It’s radiation and chemo. And it makes you really tired — which they said about chemo, but I had the steroid. I won’t have the steroid with this.
CL: So the question I hear from everybody and I’m sure you get too is ‘when are you coming back to SoulCycle?’
SG: I’m trying to wrap my head around going back to teaching. I’ve been off work since the July 4th weekend. Right now the thought of going back 30 pounds heavier, and not the same person physically and emotionally, teach to music and have to deal with other people’s feelings… it has me a bit anxious. I’ve never had clinical anxiety which I have now. I’ve never had teaching anxiety.
CL: Understandably…
SG: I’d like to go back to work when I don’t have any medication in my body for anything. I’m on so many medications right now it doesn’t feel like me. I don’t think people realize I’m responsible for everybody in the room for those 45 minutes. When you’re teaching, if anybody has an issue it’s my job to deal with it and make sure they’re okay. I want to make sure that I’m 100% ready to deal with anything that comes my way. It’s also very physical. I’m not on the bike but I don’t really stop moving, jumping, dancing, talking. But I’ll get there.
CL: It might be easier to go back on the bike.
SG: Yes, but it’s going to take me a couple of months to get back in shape — teaching shape. But with the neuropathy, there is just no way I could do that right now.
CL: You know what would be amazing is if you could teach a class with a handpicked group of trusted friends and students to start, just so you could get back in shape. We’d all respect however you wanted to lead the class. We’d just be riding together. You could say, ‘I don’t want anyone to ask me how I’m doing. Let’s just go in this room and ride the bike.’ This would be for you and I know everyone in your close circle of riders would want to be a part of that.
SG: We could definitely do that.
CL: Someone asked the other day, I mean people ask me all the time, how you’re doing. My answer has been you’re so strong, you’re going to be ok. But one person replied, she IS ok.
SG: Yes, if anyone is wondering if I’m going to be ok… I AM ok. I was never not ok.
As we finished our interview and our walk in the park, in the meadow next to The Metropolitan Museum of Art, dragonflies were buzzing all around. Stacey pointed them out to me, arm outstretched, tattooed with a dragonfly and her father’s signature underneath.
On July 3rd, 2024 SoulCycle sent this email…
Hello BARN community!
We hope you’re enjoying the Summer of SOUL at the BARN this season!
We’re reaching out to let you know that we are excited to welcome Stacey back to the SoulCycle schedule. Stacey’s first class back will be on Saturday, July 13th, 6pm at The BARN. SoulEarly booking is now open for her first classes back on July 13th and 14th. Catch her on the schedule moving forward!
See you and SG at the BARN soon!